Amyloidosis is a “group of diseases” that have the common feature where abnormal proteins (or in some cases normal proteins) behave abnormally, and the breakdown product of these proteins fold upon themselves, creating amyloid” fibrils” which deposit in various organs throughout the body. This potentially life-threatening disease can affect the heart, kidneys, liver, spleen, nervous system and digestive tract. (Falk, R., MD, 2018) A basic illustration of the creation of amyloid “fibrils” is shown below.

(Cleveland Clinic, 2020)
There are different types of the disease including AL or Light Chain Amyloidosis, AA Amyloidosis, Transthyretin Amyloidosis (referred to as TTR amyloidosis), and Localized Amyloidosis. TTR amyloidosis includes a hereditary type and a non-hereditary type. (Falk, R, MD, 2018)
Common symptoms of amyloidosis are shown in the following figure.

(The Canadian Amyloidosis Support Network)
Light Chain (AL) Amyloidosis
AL amyloidosis is the most common type of amyloidosis in developed countries, accounting for approximately 85% of all cases. There are approximately 3,000-5,000 new AL amyloidosis cases a year in the United States. (Falk, R., MD, 2018)
The disease usually affects the heart, kidneys, liver and nerves. This type of amyloidosis is blood related, associated with the abnormality of proteins from plasma cells associated with bone marrow. Plasma cells normally create antibodies, known as immunoglobulins, that serve to combat bacteria and viruses. Antibodies are made up of “heavy chains” and “light chains.” AL amyloidosis stems from an abnormal expansion of plasma cells. The abnormal plasma cells secrete abnormal “free light chains” (FLCs) into the bloodstream. These abnormal light chain mutations become “sticky.” The sticky light chains bind together to form amyloid fibrils which can then accumulate in various body organs, as shown below. (Sherwood, A.L.)

(Cleveland Clinic, 2020)
Diagnostic testing for AL amyloidosis includes blood testing, urine tests and biopsies. Blood and/or urine tests are used to indicate the presence of amyloid protein, however bone marrow tests or other small biopsy samples of tissue or organs are needed to positively confirm the diagnosis of amyloidosis. Specific types of blood/urine testing include:
- A 24-hour urine collection to look at the level of protein in your urine sample. Excess protein in the urine may be an indication of kidney involvement.
- The level of ALP (an enzyme called “alkaline phosphatase”) in your regular blood workup.
- Blood tests to look for stress and strain on the heart. Cardiac biomarkers that are used include troponin T or troponin I, and NT-proBNP (which stands for N-terminal pro-brain natriuretic peptide) or BNP (brain natriuretic peptide).
- Tests for abnormal antibody (immunoglobulin) proteins in the blood include the Free Light Chain Assay, which shows the level of kappa and lambda light chains in a separate blood test. The Free Light Chain Assay test is often referred to as FLC, which is an abbreviation for free light chains.
- Another test for abnormal immunoglobulin can be done with blood and/or urine. It is called “immunofixation electrophoresis.”
Echocardiogram and imaging are performed so that the doctor can look for amyloid deposits in the heart, while viewing the size and shape of it and the location and extent of any impact of amyloid.
Tissue biopsy are performed to identify evidence of amyloid deposits. Tissue samples are sent to a lab for microscopic examination, where the tissue is stained with a dye called “Congo-red.” After putting it under a microscope, amyloid protein is discovered if it turns an apple-green color, resulting in a diagnosis of amyloidosis. The most common tissue sample, which is almost always involved in generating an AL diagnosis, is called a fat-pad biopsy. Fat-pad biopsies are taken from the stomach. Biopsy samples may also be taken from the liver, kidney, nerves, heart, stomach, or intestines.
Bone marrow tests are also performed. These involve the removal of some liquid bone marrow and/or the removal of bone tissue. These samples can help to determine the percentage of amyloid producing plasma cells, and when tested in the lab they can assist in identifying whether the abnormal plasma cells are producing kappa or lambda light chains. (Amyloidosis Foundation, 2021)
If treatment begins during the early onset of clinical symptoms, the overall success rate is higher, so early detection is essential.
Patients with AL amyloidosis have benefited from the recent development of new drugs for myeloma, many of which work effectively on the plasma cells that cause AL amyloidosis. In addition, the FDA approved the first drug treatment specifically for AL amyloidosis in January 2021, called DARZALEX (daratumumab). Drug combinations are more effective than single drugs in attacking the abnormal plasma cells. Drugs that may be useful include traditional chemotherapy drugs (such as melphalan, and cyclophosphamide), as well as “proteasome inhibitor” and “immunomodulator” drugs. (Amyloidosis Foundation, 2021)
Stem cell transplant is also a preferred therapy, as it can provide long-term control of the underlying disease. However, only a minority of AL patients (typically less than 25%) are eligible. (Amyloidosis Foundation, 2021)
AA Amyloidosis
AA amyloidosis results from increased levels of the circulating serum “amyloid A protein.” Amyloid A protein levels normally elevate in the bloodstream as a response to infection and inflammation. If a patient has an infection or inflammatory condition for an extended period of time (six months or more) they would be at risk for developing AA amyloidosis. The amyloidosis can arise due to chronic inflammatory and infectious conditions, including rheumatic disease, inflammatory bowel disease, tuberculosis, osteomyelitis, lupus, and hereditary fever syndromes. Amyloid deposition usually begins in the kidneys, but the liver, spleen, lymphnodes, and intestines are also commonly affected.
If a patient has been diagnosed with a chronic inflammatory disease or chronic infection and they develop high levels of protein in the urine or other associated AA symptoms, then the physician should test for AA amyloid deposition. When kidney damage occurs, it can be clinically shown as protein found in the urine (nephrotic syndrome) or impairment of kidney function.
A test involving a 24-hour urine collection can be performed to look at the level of protein in the patient’s urine. If amyloidosis is suspected in most cases a biopsy of the kidney tissue performed.
In order to identify AA amyloid, the most common diagnostic test is staining the tissue sample with antibodies that are specific to AA amyloid, the “anti-AA serum.” If the anti-AA serum result is positive then AA amyloidosis is diagnosed. Once AA amyloidosis is confirmed the primary underlying inflammatory condition should then be identified.
With AA amyloidosis it is most important to treat the underlying infection or inflammation in order to reduce the level of the precursor for the AA amyloid deposits. These treatments vary depending on the underlying condition. Some treatments that exist for inflammatory diseases include surgery on the infection or tumor, drug therapies for rheumatoid arthritis, antibiotics for chronic infection, among others.
With effective treatment of the underlying inflammation amyloid deposits have been known to reduce and nephrotic syndrome can improve. If the kidney function has become significantly impaired, it rarely recovers.
Supportive treatment is very important, including nephrology, cardiology, and neurology. (Amyloidosis Foundation, 2021)
TTR (Transthyretin) Amyloidosis
As stated earlier, TTR amyloidosis includes a hereditary type and a non-hereditary type.
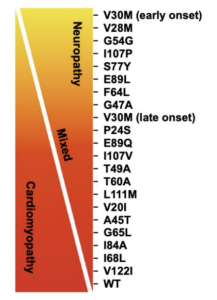
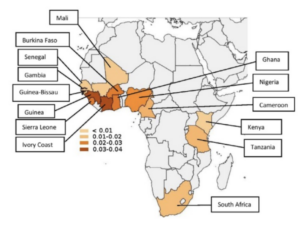
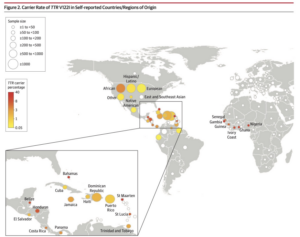
Hereditary (Familial) Amyloidosis, also referred to as ATTRv amyloidosis, is associated with an inherited genetic mutation. There are various subtypes of familial amyloidosis that are associated with specific demographic groups including Portuguese, Irish, Swedish, Afro-American, and Japanese lineage.
The non-hereditary type of TTR amyloidosis, known as Wild Type Amyloidosis is a disorder predominately of older men in their 70s and beyond. This form of the disease may actually be responsible for up to 10% of male patients having heart failure due to stiff heart tissue. (Falk, R., MD, 2018)
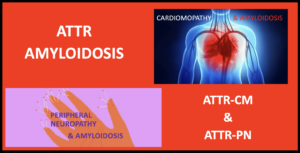
As with AL and AA Amyloidosis, TTR Amyloidosis can manifest itself with a multitude of symptoms. In a vast majority of cases the resultant symptoms are cardiological and/or neuropathic in nature. A basic illustration of the production method for TTR amyloid fibrils is shown below.

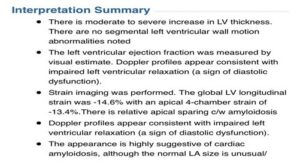
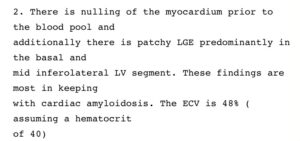
Early diagnosis if TTR amyloidosis is essential so as to help minimize the extent of bodily tissue or system damage. First, a patient is tested to determine if they have amyloid proteins in their body. The main diagnostic testing is similar to that described above for AL Amyloidosis, including blood tests, urine tests and biopsies. If amyloidosis is confirmed but the type is not initially identified, additional tests are performed to determine the existence and variation of ATTR.
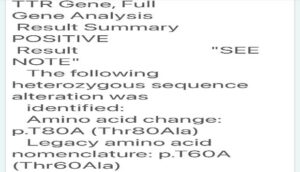
Once it is determined that there is transthyretin amyloid protein (via biopsy and Congo red staining), the specific protein needs to be identified by protein sequence analysis and DNA sequencing. A blood sample is sent to a lab where the DNA chains are analyzed. Sections of the DNA chain are checked for genetic markers of the DNA defect. Hereditary amyloidosis variations affect patients differently. It is critical to establish which variation exists in order to identify a tailored treatment plan.
Treatment of TTR amyloidosis include treating the source and symptoms. Source treatment involves slowing down, or stopping, the overproduction of amyloid at the source of the disease. Historically, liver transplant has been helpful, however, the statistics vary as to who can benefit from these transplants, with the outcome dependent largely on the specific mutation that exists in the patient. In some situations, combined heart and liver transplants have helped patients with an ATTR variant that produces cardiac problems.
In 2019, two drugs were approved for treatment of ATTR polyneuropathy associated with TTR amyloidosis in adults. The first was ONPATTRO (patisiran), a first of its kind RNA interference therapeutic drug which aims to silence the gene expression for patients with the hereditary type TTR. The second drug approved is TEGSEDI (inotersen), which reduces the production of TTR protein. Also, in 2019, VYNDAQEL and VYNDAMAX (tafamidis) were approved by the FDA for ATTR cardiomyopathy. (Amyloidosis Foundation, 2021)
There is supportive treatment for the various symptoms associated with TTR Amyloidosis, possible symptoms include peripheral neuropathy, autonomic neuropathy, cardiac and kidney problems. There are medications that can be prescribed to treat the effects of peripheral neuropathy, such as tingling or burning sensations. Many patients experience autonomic neuropathy and may require treatment for blood pressure, heart rate, digestion, and perspiration, depending on the location of the damage to the nerves. Other gastrointestinal dysfunctions may require treatment for symptoms that include poor nutritional health, diarrhea or constipation, and nausea or vomiting. (Amyloidosis Foundation, 2021)
Localized Amyloidosis
Localized amyloidosis often has a better prognosis than the types that affect one or more organ systems. Typical sites for localized amyloidosis include the bladder, skin, throat or lungs. Correct diagnosis is important so that treatments that affect the entire body can be avoided. (Mayo Clinic. 2021)
Summary
Amyloidosis is a complex multi-systemic disease where no two patients are alike. Symptoms are often vague and vary from patient to patient, even within the same disease type, making diagnosis one of the biggest hurdles for the medical community. It is not uncommon to hear from patients that it took multiple years and multiple doctors to ultimately arrive at a correct diagnosis, all the while the disease continued to progress. While treatment is type-specific, it is individualized from patient to patient depending on organ involvement.
In the words of Morie A. Gertz, M.D., M.A.C.P., of the Mayo Clinic and regarded as a leading world expert on amyloidosis.
“Thanks to the Amyloidosis Speakers Bureau, providers across the country are being instructed on techniques to suspect and recognize amyloidosis and how to efficiently make the diagnosis in a timely fashion. Incorporating testing for amyloidosis into the work flow of patients with cardiomyopathy, proteinuria, peripheral neuropathy, unexplained weight loss, and smoldering multiple myeloma has been successful.
Comprehensive education remains the best strategy to save lives for this rare disorder.”
Sources
Falk, Rodney, MD, Understanding Amyloidosis. (2018).https://www.youtube.com/watch?v=bE68vvDtnyM&t=134s.
Cleveland Clinic. (2020, June 2). Amyloidosis: AL (Light Chain). https://my.clevelandclinic.org/health/diseases/15718-amyloidosis-al-amyloid-light-chain.
Sherwood, A. L. (n.d.). Understanding Freelite®, the lab test for serum free light chains. Lecture.
Mayo Clinic. 2021. Amyloidosis – Symptoms and causes. [online] Available at: <https://www.mayoclinic.org/diseases-conditions/amyloidosis/symptoms-causes/syc-20353178> [Accessed 14 July 2021].
Amyloidosis Foundation. 2021. AL – Amyloidosis Foundation. [online] Available at: <https://amyloidosis.org/facts/al/#diagnosis> [Accessed 14 July 2021].